Ampulloma with Fluctuating Liver Tests
Case of the Week
Case of the Week
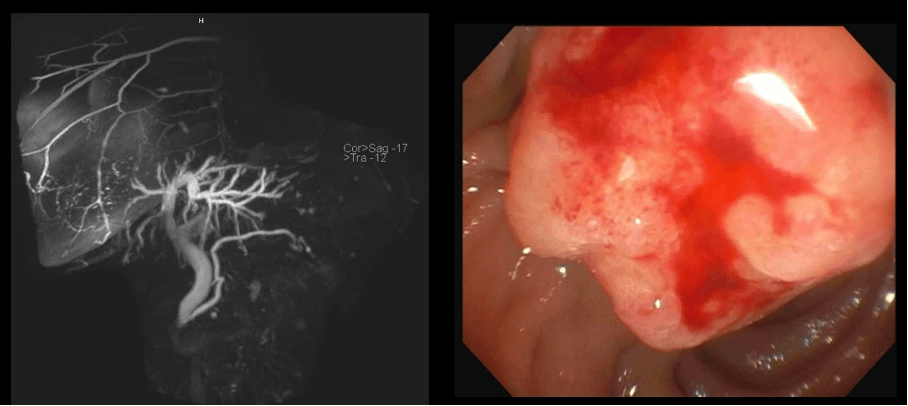
A female patient in her late 70’s with status post cholecystectomy and a history of breast cancer on anastrozole, which was stopped 1 month prior because of itching was found to have elevated liver tests (alkaline phosphatase up x 4, ALT up x 6, AST up x 4). MRCP showed dilated common bile duct to 11 mm with smooth tapering at ampulla of Vater. The patient was sent for EGD and endoscopic ultrasound (EUS). The liver tests had decreased by 50% on the day of the procedure. The ampulla had the above appearance on EGD with a distal cap. What would you do next?
Approach described by Dr. Fateh Bazerbachi:
We opted for an ERCP first, given the higher risk of EUS-FNB induced pancreatitis without a protecting prosthesis and lower perceived risk of intraductal and ampullary sampling following sphincterotomy to separate the PD and CBD orifices.
The selective cannulation was aided by waiting for a hint of bile to aim for the CBD opening given that landmarks were not clear with the ulcerated surface of the ampulla.
The issue with pure EUS core sampling and mucosal biopsies is risk of ampullary hematoma, biliary obstruction and pancreatitis.
Further, with the appearance noted in this case, and relatively small lesion, yield of core biopsies with 22G needle will be limited, and pancreatitis with 19G sampling is a high risk (many experts would quote same risk of pancreatitis as ampullectomy when large caliber FNB is used in this location). Lastly, with highly suspicious endoscopic appearance of the lesion, a negative round of sampling is not sufficient to stop the evaluation. Hence, biliary prosthesis placement is a reasonable approach. As we see in this case, sampling was not conclusive and best next step is to repeat biopsies vs proceeding with ampullectomy as a diagnostic and therapeutic technique with PD stent placement (imperative) given age and comorbidities, I favor the former. If this is negative then shared decision making with the patient and ampullectomy would be the next step in my opinion.


