Gastrointestinal Bleeding due to Amyloidosis
Investigating the Intersection of Rheumatoid Arthritis, Gastrointestinal Bleeding, and Amyloidosis
By Klaus Mönkemüller MD, PhD1-3, Frank Aedtner, MD1, Adrian Canavesi, MD2
1Department of Gastroenterology, Helios Frankenwaldklinik, Kronach, Germany
2Department of Gastroenterology “Prof. Carolina Olano”, Hospital de Clínicas, Universidad de la República, Uruguay
3Department of Gastroenterology, Virginia Tech Carilion School of Medicine, Roanoke, USA
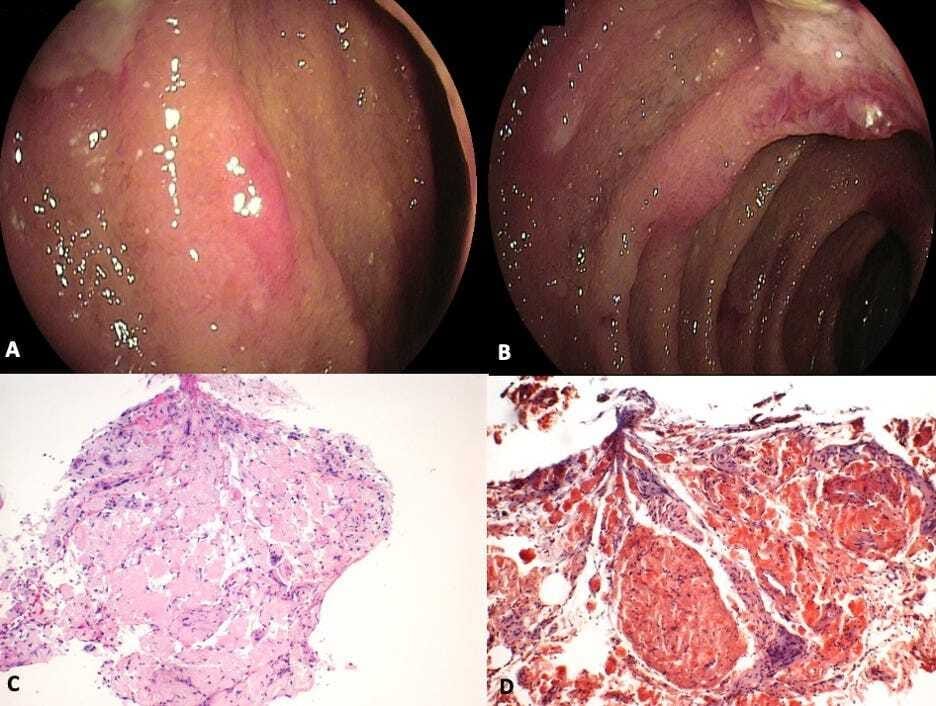
An elderly female patient with long history of rheumatoid arthritis presented with hematochezia for 3 days. Both EGD and colonoscopy were unrevealing. On deep enteroscopy a large segment of edematous and ulcerated mucosa with multiple areas of pink-violaceous discoloration, submucosal hemorrhages, and friability were seen in the proximal jejunum (Panels A and B). Histology revealed submucosal depositions of amyloid (Panel C) The Congo red-staining in polarized light confirmed amyloid depositions (Panel D). A systemic distribution of amyloidosis was further confirmed by finding amyloid deposits in additional, deep biopsies obtained from stomach and duodenum.
Amyloidosis is the process of protein fibril deposition in the extracellular space of tissues and organ systems. Over 20 different proteins are known to form amyloid fibrils but not all of this cause disease (1). The majority of amyloidosis can be categorized into two main subtypes, amyloid light chain (AL) and amyloid A protein (AA). AL amyloid is a manifestation of a primary plasma cell dyscrasia encompassing the spectrum of multiple myeloma (MM), smoldering multiple myeloma (SMM), monocolonal gammopathy of undetermined significance (MGUS), and primary amyloidosis. Fifteen percent of AL amyloid patients have multiple myeloma (2). AA amyloid occurs as a response secondary to systemic inflammation such as rheumatologic disorders, inflammatory bowel disease, and tuberculosis. The manifestations of amyloidosis vary depending on the site and extent of the protein deposition. Of the known types of amyloidosis to cause disease, including systemic AA amyloidosis, β2-microglobulin amyloidosis, hereditary systemic amyloidosis, and senile systemic amyloidosis, AL amyloidosis is observed to incur the most GI involvement.
This case highlights the importance of performing deep enteroscopy in patients with obscure gastrointestinal bleeding and always think of amyloidosis as a potential etiology of ulcerative small bowel diseases, especially in patients with chronic inflammatory conditions, or blood dyscracias such as multiple myeloma (3,4).
Amyloidosis on EndoCollab
EndoCollab
✅ 1000+ endoscopy strategies
✅ 900+ endoscopists
✅ EndoCollab community to ask your questions
✅ No obligations, no contracts, CANCEL ANYTIME

References:
Ebert EC, Nagar M. Gastrointestinal manifestations of amyloidosis. Am J Gastroenterol 2008;103:776-787.
Menke DM. et al. Symptomatic gastric amyloidosis in patients with primary systemic amyloidosis. Mayo Clin Proc. 1993;68:763-767.
Tada S, Iida M, Yao T, Kawakubo K, Yao T, Okada M, Fujishima M.Endoscopic features in amyloidosis of the small intestine: Clinical and morphologic differences between chemical types of amyloid protein. Gastrointest Endosc 1994;40;45-50.
Gono T, Matsuda M, Dohi N, Sekijima Y, Tada T, Sakashita K, Koike K, Kadosaka S, Ikeda Si. Gastroduodenal lesions in primary AL amyloidosis. Gastrointest Endosc 2002;56:563-5.

