Angiodysplasias of the “Cecum” and Aortic Stenosis: Heyde's Syndrome
A big thank you to this week's sponsors who help keep this newsletter free for the reader:
EndoCollab: Connect with other gastrointestinal endoscopists and expand your knowledge with EndoCollab. Our online community offers discussion forums, on-demand video courses, and daily tips to help you stay up to date in the field. With over 800 members, you'll have access to a wealth of experience and expertise. Join EndoCollab today and be a part of our growing community. Join EndoCollab.
The classic teaching refers to Heyde’s syndrome as “the association of aortic stenosis and cecal angiodysplasias”. Whereas this is partially true, in this newsletter you will learn that Heyde syndrome is a type of hemophilia (acquired von Willebrand disease) leading to GI bleeding from various types of gastrointestinal angiodysplasias.
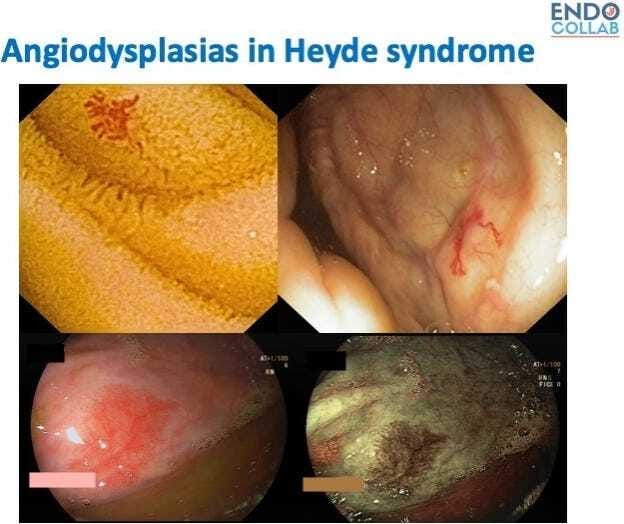
As you can see from the images (Figure 1), angiodysplasias in Heyde’s syndrome can happen anywhere in the gastrointestinal tract, and not only in the cecum as commonly believed.
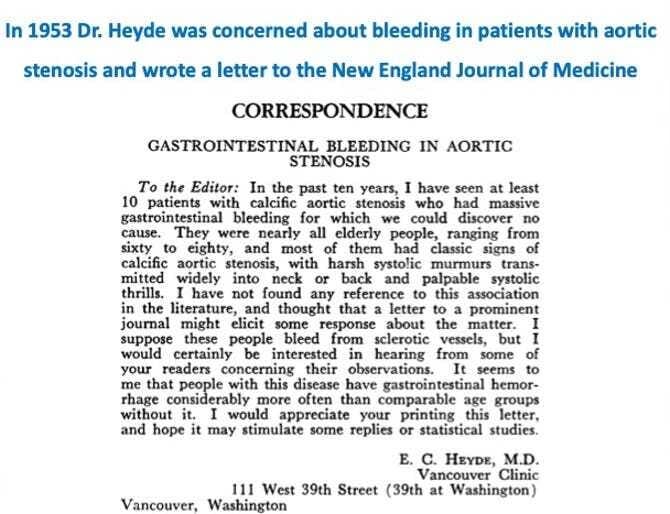
Indeed, Dr. Heyde never specifically mentioned the cecum as the source of bleeding (1). He observed that patients with aortic stenosis had cryptogenic bleeding, speculating that it might originate in “sclerotic vessels”. His astute observations, manifested in simple letter to a medical journal (Figure 2, reference No.1), opened a pandora’s box trying to elucidate the association of aortic stenosis and gastrointestinal bleeding.
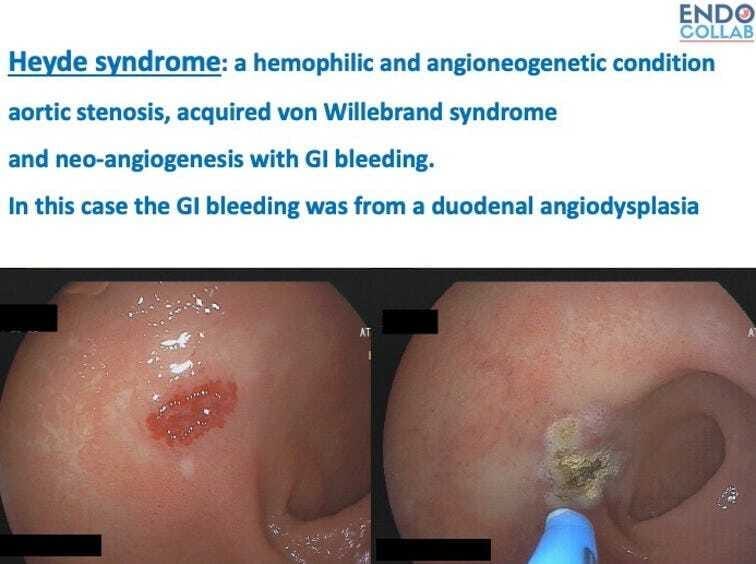
Much has been learned from Heyde syndrome over the last decades and now we know that it is primarily a hemophilia, namely a form of acquired von Willebrand syndrome (2-4). There is a malfunction of von Willebrand factor, leading to gastrointestinal hemorrhage. In addition, deranged von Willebrand activity leads to angioneogenesis and occurrence of angiodysplasias in the GI tract (2-4) (Figure 3).
How does von Willebrand factor malfunction in Heyde syndrome?
- The malfunction of von Willebrand factor is indeed initiated by the abnormal blood flow from aortic stenosis.
- This abnormal blood flow results in increased shear forces, which led to destruction of the normally circulating (or folded, globular) von Willebrand factor, which is unfolded, exposing its center to the destructive or catalytic enzymes ADAMTS 13.
- Inactivation of von Willebrand factor leads to a bleeding state.
- Another important pearl is that lots of other cardiovascular conditions, in addition to calcific aortic stenosis may lead to Heyde syndrome. These include HOCM, single ventricle or implanted left ventricular assist devices (LVAD).
For those interested in deeper understanding of this hemophilic condition I have summarized the pathophysiology (4,5).
- von Willebrand Factor (vWF) is a large multimeric glycoprotein, present in blood plasma, endothelial cells, megakaryocytes, and platelets.
- von Willebrand factor (vWF) is a produced in the endothelial cells and stored in the storage granules of these cells, which are called Weibel-Palade bodies.
- Von Willebrand factor plays a major role in hemostasis, mediating platelet adhesion to vascular injury sites.
- Von Willebrand factor also carries factor VIII, which it binds and protects from degradation.
- Von Willebrand factor is released as folded or globular heterodimer into the circulation.
- Flow acceleration and deceleration in aortic stenosis, and other cardiac conditions with deranged flow states (such as left-ventricular assist device-LVAD, hypertrophic obstructive cardiomyopathy - HOCM), result in unfolding of von Willebrand factor, which loses its thrombotic activity.
- In the absence of von Willebrand factor, FVIII is unstable and exposed to rapid degradation.
- The unfolded form of von Willebrand induces angioneogenesis through Ang2 and vascular endothelial growth factor (VEGF).
- Development of angiodysplasias (due to neo-angiogenesis) is further induced by hypoxia and low flow states
In summary, Heyde syndrome is an acquired von Willebrand disease. The defective von Willebrand factor is a decisive factor leading to hemorrhage due due defective platelet adhesion and angiogenesis and angiodysplasias of the gastrointestinal tract, which in turn bleed due to their inherent deformation and frailty and as a result of the acquired hemophilia.
The trigger for this acquired hemophilia are a wide spectrum of cardiovascular conditions such leading to abnormal blood flow with high shear forces, which destroy the normal von Willebrand factor in the circulation. These conditions include aortic stenosis, hypertrophic obstructive cardiomyopathy and left-ventricular assist device, among others. Importantly, correction of the underlying cardiac condition often leads to resolution of Heyde’s syndrome.
Importantly, treatment consists of correcting the low-flow state with high shear forces, e.g. replacement of the aortic. This aids in the resolution of the problem in the vast majority of patients.
References:
1. Heyde, E.C. Gastrointestinal Bleeding in Aortic Stenosis. N. Engl. J. Med. 1958, 259, 196.
2. Warkentin, T.; Morgan, D.G.; Moore, J.C. Aortic stenosis and bleeding gastrointestinal angiodysplasia: Is acquired von Willebrand’s disease the link? Lancet 1992, 340, 35–37.
3. Warkentin, T.E.; Moore, J.C.; Morgan, D.G. Gastrointestinal Angiodysplasia and Aortic Stenosis. N. Engl. J. Med. 2002, 347, 858–859.
4. Vincentelli A et al. Acquired von Willebrand in Aortic Stenosis. New Engl J Med. 2003
5. Okhota S, et el. Int. J. Mol. Sci. 2020, 21, 7804;


Hi Klaus:
Excellent review 👍💪👊👌
Hug,
Nadhy
Thank you much Nadi 🙏🏻😃