Clostridioides Difficile Infection (CDI)
A Comprehensive Summary with Quick Facts for Your Practice
Pathogen:
- Anaerobic, gram-positive, rod-shaped bacterium with spore formation
- Spores have tolerance to heat, desiccation and many disinfectants.
- Two exotoxins: toxin A (“enterotoxin”) and toxin B (“cytotoxin”)
- Careful: the hypervirulent strain: NAP-1,ribotype 027, III has increased expression of toxins A and B.
Risk Factors:
- Main risk factors: previous antibiotic therapy, hospitalization, age > 65 years
- Other risk factors: multimorbidity, female, H2 and PPI therapy, immunosuppression
Definition of infection: symptoms plus evidence of toxins A and B
- Watery diarrhea or toxic megacolon (occasional no diarrhea in paralytic ileus!)
- Blood in stool (rare), abdominal pain (22%), fever (28%), peritonitis/ascites
Laboratory findings:
- Leukocytosis (>15,000/µl (50%), hypoalbuminemia, creatinine increase ≥1.5 times, lactate increase
Diagnostics (Attention: only perform diagnostics on patients with clinical symptoms of CDI!)
- antibiotics in the last 60 days; risk groups, regardless of whether they are hospitalized, and any diarrhea lasting more than three days without other known pathogens
- Stool samples
- EIA test (quick but only 80% sensitive).
- GDH, if positive then toxin, then PCR.
- Imporant: fresh stools, max. 2 hours transport time (toxin breaks down at room temperature, no rectal swabs!). Culture rarely helpful (too high TAT, turn-around time)
- Cytotoxicity test (cell culture-based method): highly sensitive and specific for toxin B
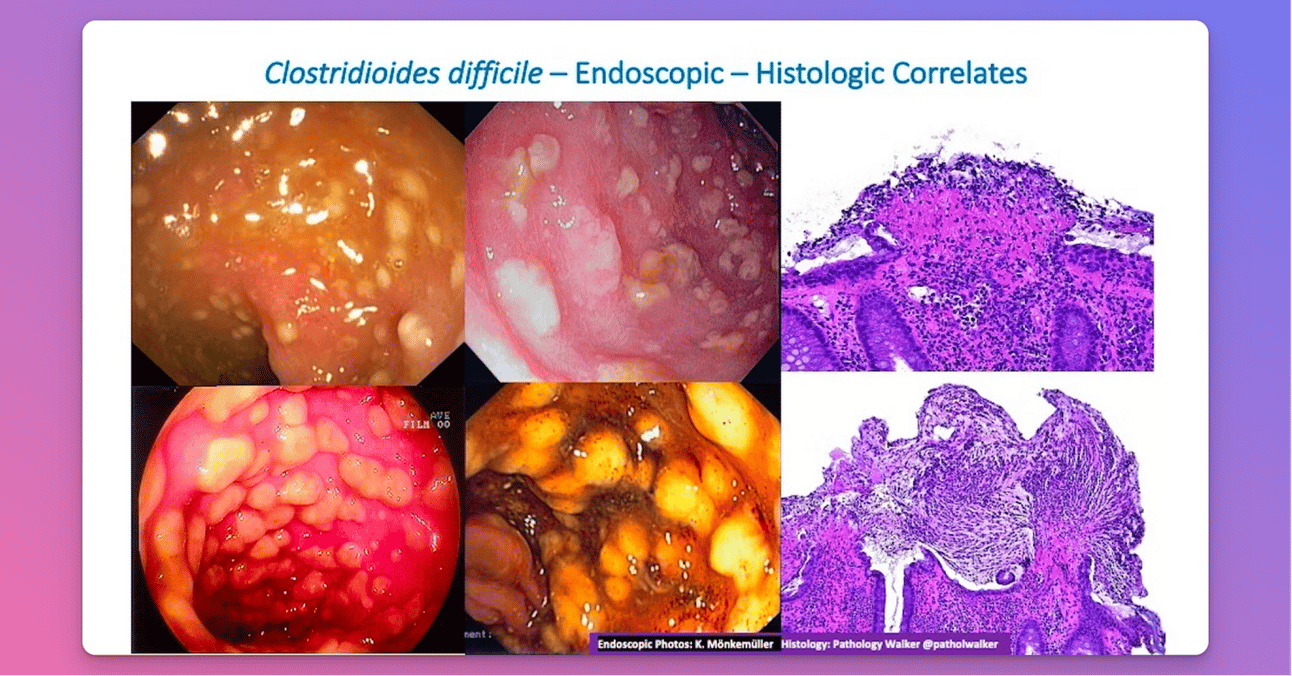
- In the absence of toxin detection DO a sigmoidoscopy: pseudomembranes = pathognomonic)
- Check-ups: only if symptoms re-appear after successful therapy, not if there are no symptoms after therapy
Classification of severity (risk stratification according to Zar, Clin Infect Dis 2007) (severe course > 2 points!)
- 1 point: > 60 years, temperature > 38.5 C, albumin < 2.5 mg/dl, leukocytes > 15,000/µl
- 2 points: endoscopic evidence of pseudomembranes, stay on ICU
Hygienic measures and therapy:
- Isolation (single room): Patient with severe diarrhea, poor compliance.
- Isolation measures should be maintained for a period of 48 hours after diarrhea has resolved.
- Disposable protective gown and hand hygiene: washing hands, then disinfection if gloves were worn: disinfection alone is sufficient, mouth and nose protection only if aerosol formation and splashing
- Adequate fluid and electrolyte replacement
- Antibiotics when: a) severe or persistent symptoms (i.e. all hospitalized patients), b) elderly and/or patients with underlying medical conditions, or c) concomitant antibiotic treatment
- Non-severe course (i.e. outpatient): metronidazole (3 x 400 mg orally or 3 x 500 mg i.v.) x 10 to 14 days.
- In the hospital, or severe course or pregnant: vancomycin orally or nasogastric tube (4 x 125-500 mg) x 10 days, and as an enema (4 x 500 mg in 100 ml NaCL; in transit disorder: metronidazole 3 x 500 mg IV vancomycin
- Intolerance: Dificlir (Fidaxomicin) (2 x 250 mg)
- Life-threatening clinical pictures (pseudomembranous colitis, toxic megacolon - TMC): combined therapy with vancomycin (oral or via enteral tubes) and metronidazole (i.v.)
- First recurrence: same as first therapy. From the second recurrence: vancomycin in tapering doses: 4 x 125 mg x 14 days, 2 x 125 mg x 7 days, 1 x 125 mg x 7 days, 1 x 125 mg/2-3 days x 2-8 weeks
Surgery consult: > 65 years, leukocytes > 20,000 µl, sepsis, TMC, severe ileus, peritonitis, perforation

