Device Review: How to Place a Rectal Decompression Tube Through-The-Scope
by Diana Dougherty, MD and Klaus Klaus Mönkemüller, MD, PhD, FASGE, FJGES
Department of Gastroenterology, Carilion Memorial Hospital, Virginia Tech Carilion School of Medicine, Roanoke, USA
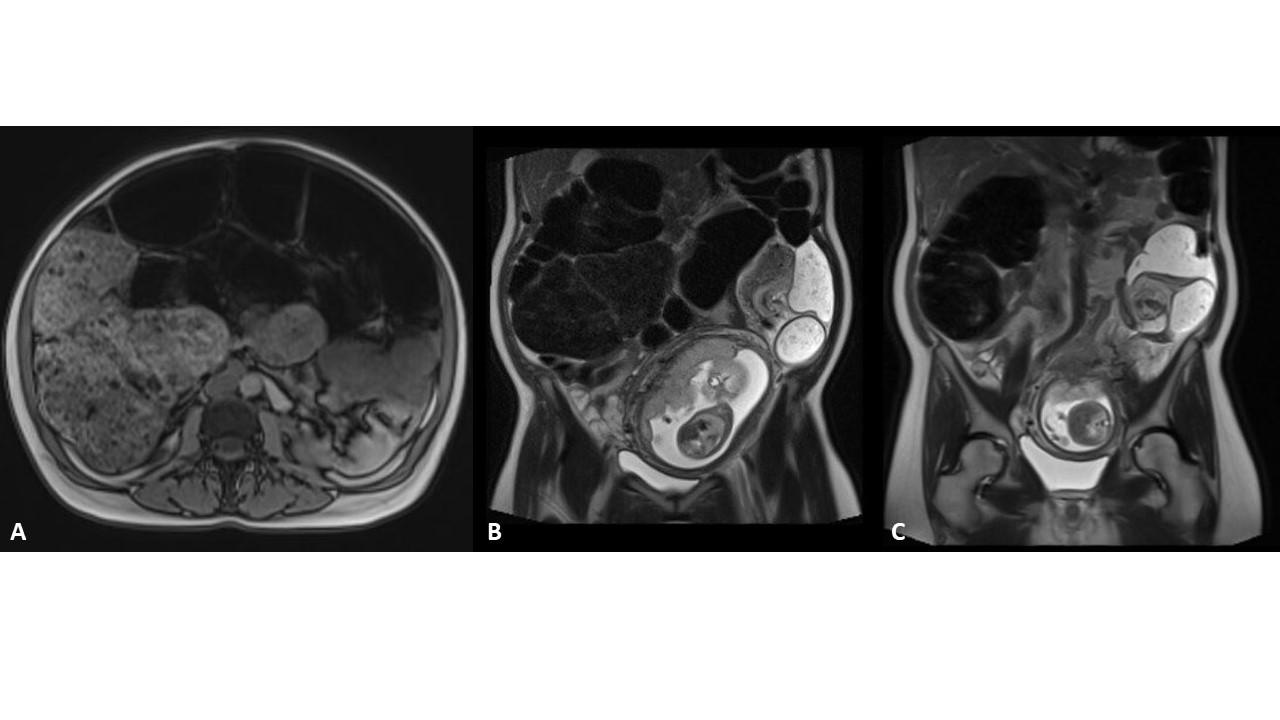
A 40-year-old pregnant woman presented with acute constipation and abdominal distention. A sigmoid volvulus was diagnosed (Figure 1). There was a transition point in the sigmoid colon with a “mesenteric swirl sign” (Figures 1B, 1C).
An emergency colonoscopy was performed to resolve the sigmoid volvulus and place a decompression tube.
Colon decompression tubes are used for other conditions such as Ogilvie’s syndrome and megacolons. In this case we used a Marcon colon decompression set (see below, Figures 2 and 3). This tube-set is particularly practical and useful as it comes with a wire and the tube has a pigtail end. This pigtail configuration prevents damage to the mucosa or colon perforation once the tube has been placed and is left inside. In addition, the tube has many side holes that allow for passage of liquid stool and air (Fig. 1 and 3D).
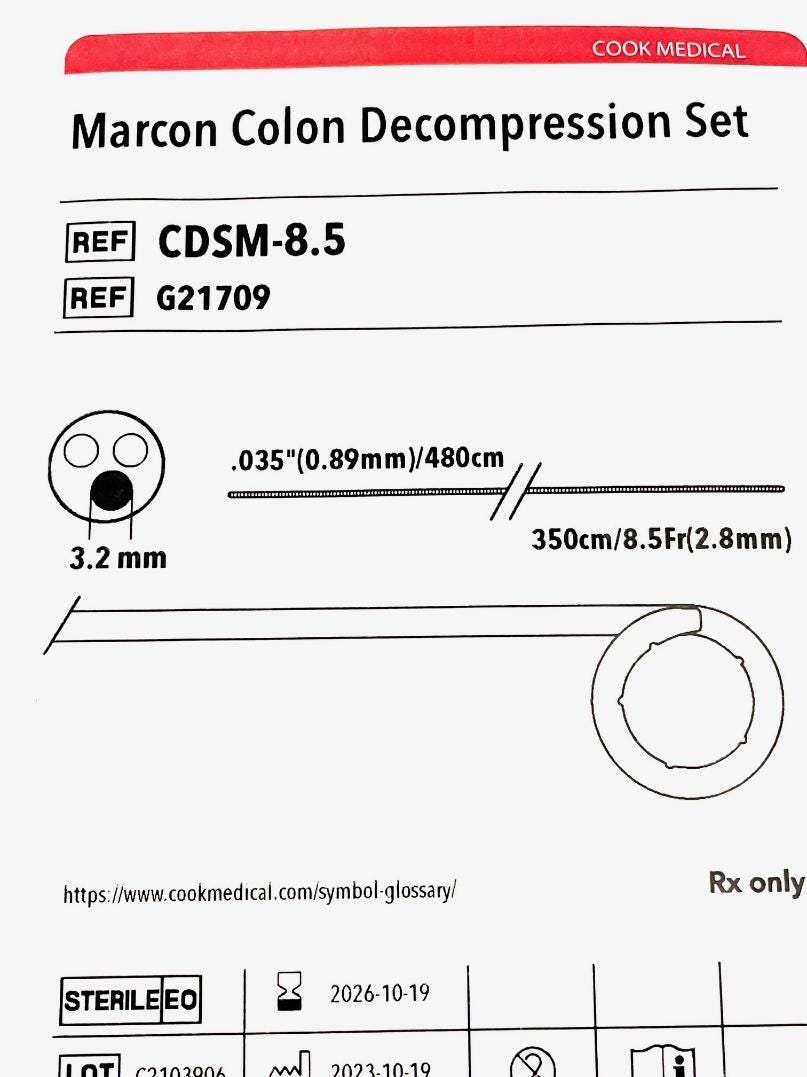
Figure 2.
The key steps to deploy place a through-the-scope colon decompression tube are:
Know your equipment. As the tube is placed through the working channel of the scope, it is imperative to have a colonoscope with a channel large enough to accept the tube. Tubes with diameters of 8.5 Fr and 10 Fr require a 3.2 mm working channel. Larger diameter tubes cannot be placed through the endoscope!
First, feed the wire into the decompression tube (Figures 1E and 1F). This wire will “stiffen the tube and facilitate pushing it through the scope channel.
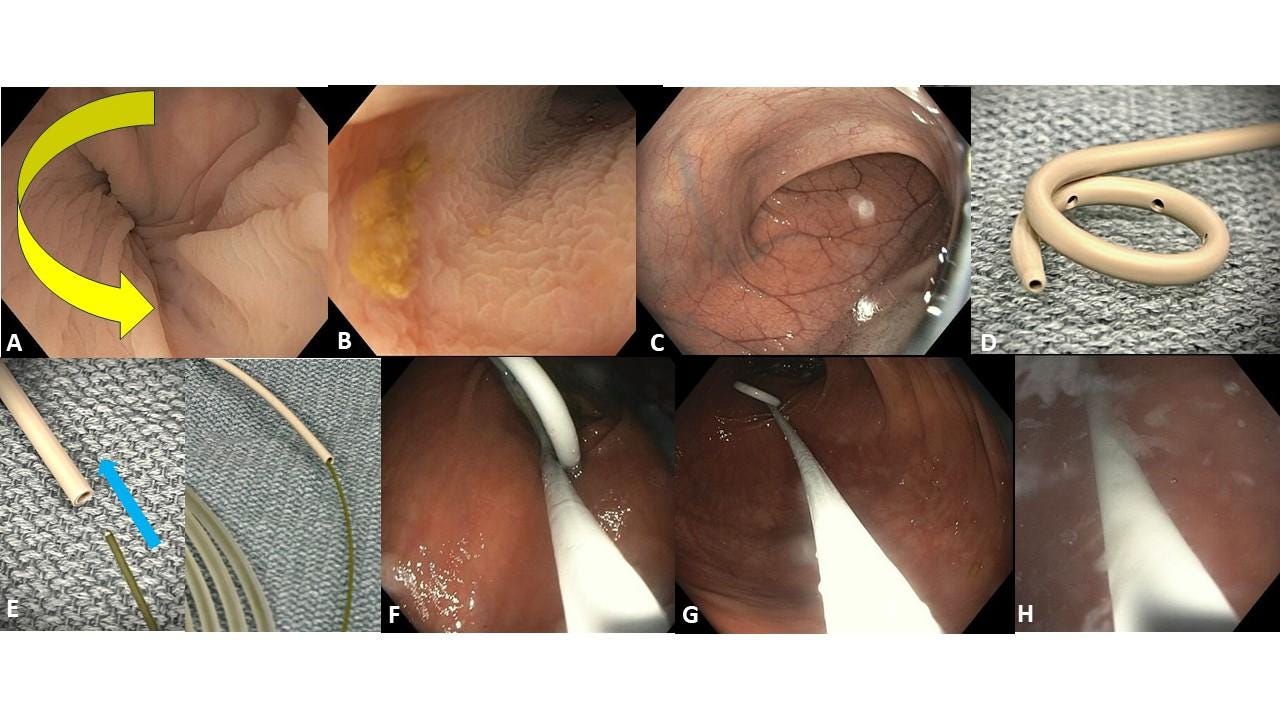
Once a location has been chosen to deploy the decompression tube, the tube is pushed out under direct endoscopic visualization until it the pigtail “coils” (Figure 1F). One trick we used to allow for smooth pushing of the catheter is to inject some olive oil into the working channel of the scope. Injecting water is also an option. It is important to always keep the wire INSIDE the catheter and not push the wire outside the pigtail tip, as the wire can penetrate the mucosa or even cause perforation. In addition, often there is liquid or solid stool that limits visualization, and a ‘free” wire tip can be dangerous.
Figures 3G and 3H shows the exchange maneuver. The catheter is pushed out and the scope is removed (by the endoscopist or an assistant). The important aspect is to advance tube and pull scope out in a synchronized matter (exchange), as you do not want to pull the catheter out. A trick we used while pushing the catheter is to start gently and slowly removing the wire. Some experts like to remove the wire at the very end, but this can lead to catheter entanglement and sometimes the wire is “stuck” inside the decompression catheter. This can result in accidentally pulling the catheter out when trying to dislodge the wire.
Figure H shows the final tip. As mentioned above we like to flush the colon with lots of water, but in distended colons we also use lots of simethicone. This will decrease bubbles and, of course, gas.
No COI by DD or KM with any of the companies/utensils or products mentioned in this article.
Advance your endoscopy practice in minutes a day
Join EndoCollab, featuring 1,000 + strategy videos, a growing atlas of real-world cases, and a private network of 1,300 + endoscopists who will crowd-source answers to your toughest questions.
Choose a flexible monthly or yearly membership—or lock in lifetime access (bonus WhatsApp group included) and cancel anytime.
Ready to level-up your skills and patient care? [Join EndoCollab now]
Download the PDF of This Article
Device Review_ How to Place a Rectal Decompression Tube Through-The-Scope.docx.pdf
467.52 KB • PDF File

