Endoscopic Resection of LST in Ascending Colon
Diana Dougherty, MD and Klaus Mönkemüller, MD, PhD, FASGE, FJGES
Department of Gastroenterology, Carilion Memorial Hospital, Virginia Tech Carilion School of Medicine, Roanoke, USA
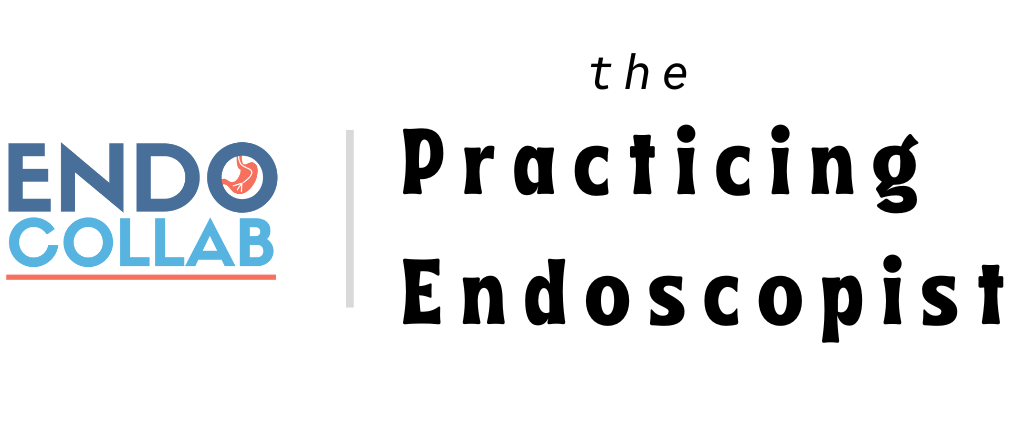
A flat polypoid lesion was found in the ascending colon (A). As this lesion was larger than 10 mm, by definition it’s an LST (laterally spreading tumor).
The key initial steps to plan an adequate resection are to:
a) determine its location (B. here we see that it is between two folds),
b) analyze its morphology (LST-granular, G), and
c) analyze its surface using close-up view with high-definition white light (C) and NBID). The mucosal pit pattern is regular, cerebroid, without ulcers or depressions (Kudo IIIL). The vessels are regular and without deformities.
d) not "loose" the polyp from sight! Pearl: Notice on image B that there is a "suction" mark. This trick is especially useful in patients whose colon is moving a lot, there is remaining debris in the colon, or the polyp is located in a difficult location. The suction mark helps find the polyp again! See the next figure for details on the suction mark technique.
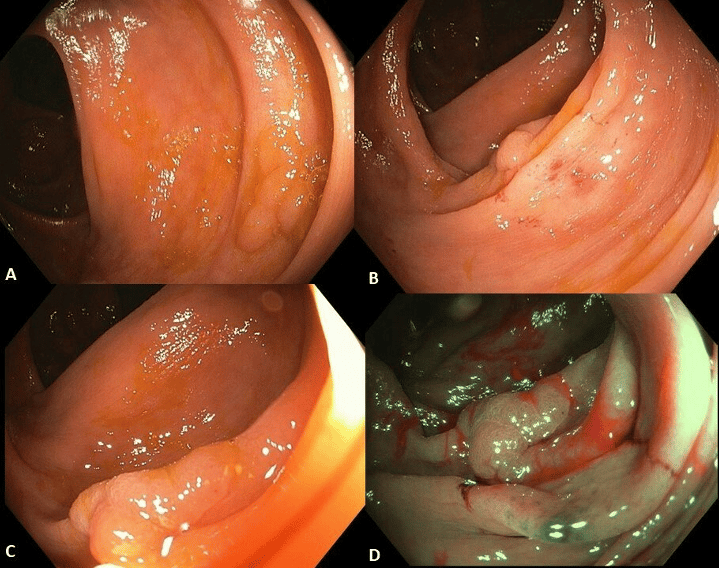
How to do the suction mark trick? Focus on the lesion, push the scope towards it and suction the mucosa right next to it. This creates a red submucosal suction mark (yellow arrows), which then becomes pivotal to re-identify or relocate the polyp (yellow circle).
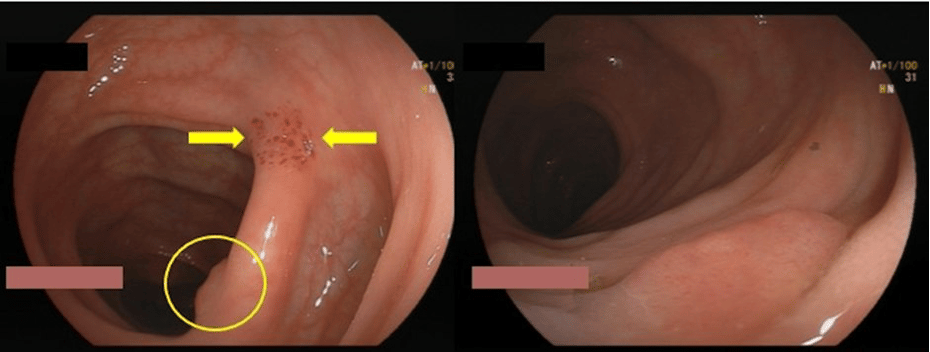
There are many ways of dealing with this flat lesion. Some experts like "cold snare", others go directly for hot snare. We prefer endoscopic resection using interventional chromoendoscopy for the following reasons: a) the LST has an irregular, almost triangular shape, b) the LST is located in-between folds, and c) we always aim at R0 (surgical or oncologic resection) and prefer not be "burning" or ablating incompletely resected borders.
By raising the LST using submucosal injection with blue color (in this case we used Eleview, Cosmo Technologies, Ireland and Germany, but you can use normal saline mixed with Indigo carmine or methylene blue or other hydroximethylcelluose such as Blue Eye) (A). Note two important aspects: a) the LST is nicely raised, well separated from the deeper layers, now the polyp is more "sessile" than flat, and b) the blue color injection clearly helps differentiate normal from pre-neoplastic or neoplastic tissue, as the color mainly depicts normal tissue. This is the concept of "interventional chromoendoscopy", when colorings are helpful to guide the endoscopist in therapeutic interventions, in this case aiming at R0 (complete resection).
Once the snare is pushed out it's used twofold, a) to calculate the size of the lesion (here the snare is 15 mm, braided, Captivator, Boston, USA) (B). The LST is thus about 12 mm in size. The submucosal cushion allowed for nice entrapment of the entire LST above the snare (C). One trick that we use is to tightly close the snare, almost aiming a "cold" resection, and applying electrosurgical current (C). Note the resection site (D). It's an endoscopic R0, exactly what we aimed at. Furthermore, by applying HOT snare technique there is a burned base and lateral margins. This ensures that no vertical or lateral tissue is left. This does not occur during COLD snaring, and it is the reason for higher adenomatous polyp recurrent rates seen after cold snare techniques.
This LST was in the right colon. The patient has hypertension. Both are risks for post-polypectomy bleeding. Therefore, we used prophylactic clips (E). Some experts would argue that clipping is not necessary. We disagree, because a) this patient had two risk factors for post-polypectomy bleeding, and b) this is an outpatient procedure, and the patient comes from a long distance. We always aim at performing "personalized" endoscopy and rely less on guidelines that may not take into account individual patient aspects, such as risks and social aspects, including distance to home, availability o emergency room close to their home and emergency endoscopy services.
When placing a clip remember two things: a) try not to insufflate the colon with CO2 or air, so that they are to be clipped remains small (figures 3D, E). After clipping use a little air to see how well the clip was placed.
No COI by DD or KM with any of the companies/utensils or products mentioned in this article.

EndoCollab. EndoCollab is an online community for GI endoscopists. With 1200+ members, endoscopists discuss interesting cases, view on-demand video courses, and get new endoscopy tips every day. Join EndoCollab
🤔 What defines a lesion as an LST (Laterally Spreading Tumor)?
A. A lesion smaller than 10 mm

