Endoscopic Therapy for Bleeding Gastroesophageal Varix (GOV 2)
by Hiral Patel, MD and Klaus Klaus Mönkemüller, MD, PhD, FASGE, FJGES
Department of Gastroenterology, Carilion Memorial Hospital, Virginia Tech Carilion School of Medicine, Roanoke, USA
A 45-year-old woman with history of cirrhosis presented with acute onset hematemesis and hypotension. After hemodynamic stabilization an urgent EGD was performed (Figure 1).

Figure 1. Gastroesophageal varix GOV 2. A. Z-line and cardia. B. Bleeding varix at the distal cardia, towards the greater curvature (GOV 2). C. Small nipple sign. D. Close up look of varix with recent stigmata of bleeding. E. During retrieval of scope the nipple sign can be clearly seen (yellow arrow). F. Endoscopic band ligation (EBL) of GOV 2. G. Effective EBL. H. Effective hemostasis after EBL.
The key steps for effective endoscopic hemostasis of gastroesophageal varices are:
Define exact location of the varix or varices. Figure 1 A. shows clear visualization of the gastroesophageal junction. Afterwards, careful retroflexion is mandatory, ideally with a clean stomach fundus. All excess blood or blood clots must be removed. In addition, we utilize simethicone to remove any bubbles.
Dynamic inspection of the lesion (panels B, C and D). During “dynamic” inspection we focus on the tissue composition, elasticity, appearance and bleeding. Generally, GOV may be treated with elastic bands (1) (Figure 2, ref 1). However, varices with lots of fibrosis (stiffness) should be treated with injection. This varix was “soft” appearing and a decision to use bands was taken.
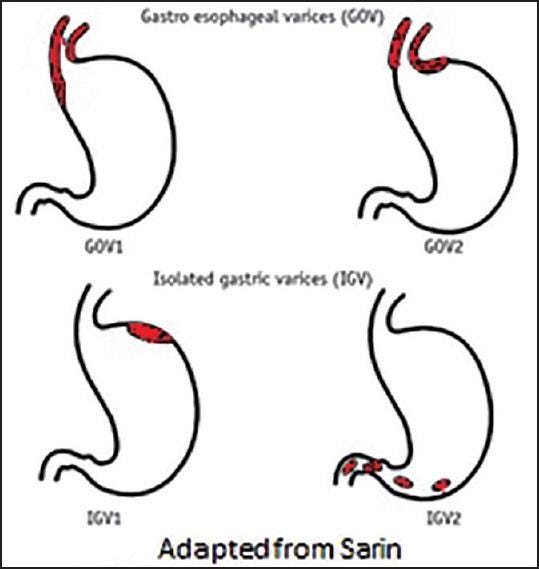
Figure 2. Sarin classification of gastric varices (1).
Inspection should also be performed in antegrade view. During inspection it is also important to determine whether there are signs of variceal rupture (i.e. “nipple” sign, panels D and E, yellow arrows) or vessel wall thinning (i.e. red spot or red wale signs). In this case, the nipple sign helped us clearly differentiate the high-risk varix from another varix in proximity (which occasionally may be banded erroneously, green arrows, panels D and E). Thus, these bleeding stigmata are important signs to relocate the varix when using the scope is reinserted with endoscopic band ligation device (cap with bands).
Although EBL may be performed in retroflexion, elastic bands are best placed in forward (antegrade) view (panel F). While suctioning the varix into the cap with bands it is essential to keep the high-risk stigmata (in this case the nipple or fibrin plug) in the center. Once the varix is about two-thirds into the cap the band must be released (“fired”). During suctioning there will be rupture of the nipple sign (fibrin plug) and bleeding will ensue. Don’t panic and don’t take your finger from the suctioning button. Instead, keep a cool head and fire the band. Soon after releasing the band stop suctioning and apply a little bit of air or even touch of water (through the water channel of the scope). This will gently push away the banded varix from inside the transparent cap and you will observe the result – a nicely strangulated varix (G, H).
References:
Wani ZA, Bhat RA, Bhadoria AS, Maiwall R, Choudhury A. Gastric varices: Classification, endoscopic and ultrasonographic management. J Res Med Sci. 2015 Dec;20(12):1200-7. doi: 10.4103/1735-1995.172990. PMID: 26958057; PMCID: PMC4766829.
No COI by HP or KM with any of the companies/utensils or products mentioned in this article.

