Giant Prolapsing Gastric Polyp
Case of the Week
Case
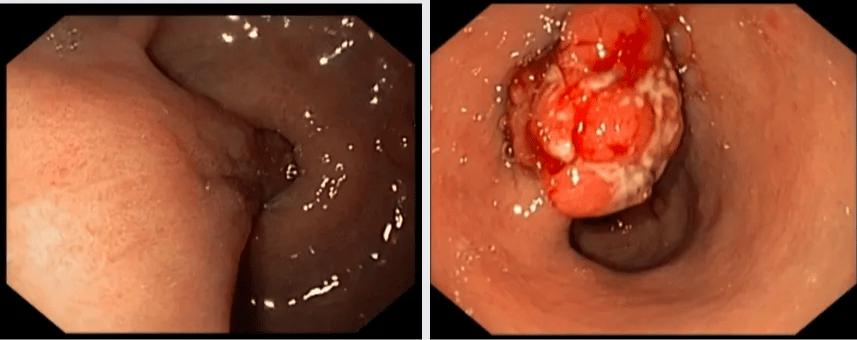
A 75-year old male with iron deficiency anemia underwent upper endoscopy. A pedunculated lesion prolapsing into the bulb across the pylorus was found. With some difficulties the lesion was "brought back" into the stomach and the head of the tumor had ulcerated surface with contact bleeding.
Since the patient was currently on ASA and clopidogrel, several biopsies were taken. He is probably a poor surgical candidate. CT scan was negative for enlarged regional lymph nodes and distant metastases.
Would you consider endoscopic removal in such case hoping for negative resection margin, despite ulcerated surface and iron-deficiency anemia indicating malignant transformation or send him for surgery? What factors would affect your decision for this lesion?
Analysis of Case
This giant prolapsing polyp is likely hyperplastic. The other important differential diagnosis is inflammatory polyp, especially the so-called Vanek tumor. Less commonly, these lesions are mesenchymal or lymphoid in origin or are cancerous (e.g. adenocarcinoma).This polyps result in intermittent obstruction and anemia or frank GI bleeding. Because of the constant prolapse their surface erodes and becomes „ugly-looking“, mimicking malignancy. If the polyps are hyperplastic, they have more chances of harboring malignancy if larger than 10 mm.This polyp is definitely > 10 mm.What would make me resect this lesion endoscopically?1. The polyp has a nice base and a long stalk (it’s more of an elongated base, due to constant bouncing back and forth).2. This nice base allows for nice submucosal injection of saline-epinephrine mix.3. The location is also ideal for controlled resection.4. If the lesion is resected and no malignancy is found or if the submucosal invasion is minimal and the margins are broad (R0), the patient is cured. And also cured from the bleeding. If there is invasive tumor, the resection was also helpful for diagnostic purposes and further therapeutic planning.5. This lesion is ideally resected using ESD or ESD-Hybrid technique. I would not proceed with a polypectomy as the stomach is highly vascularized and these lesions tend to harbor huge vessels. The risk of bleeding would be too high. That’s why performing a controlled resection, step-by-step is better.6. Pre-resection endoscopic ultrasound is highly recommended. EUS may be very helpful determining infiltration. If there is deep infiltration I would not resect endoscopically. In the absence of EUS I would do a CT of the abdomen, if the kidney function is fine.
Case presented by Dr. Stefan Mitev and discussed by Prof. Klaus Mönkemüller


Can we perform clipping or endoloop then snare polypectomy?
great case. have resected this large pedunculated HP prolapsing into pylorus causing partial gastric outlet obstruction with endoloop. I counsel the patient that they have potential to recur later but the benefit of resecting the polyp now outweight the risk of recurrence of the polyp. Is surveillance on a yearly basis be recommended?