How Does Clostridioides Difficile Lead to Massive Leukocytosis?
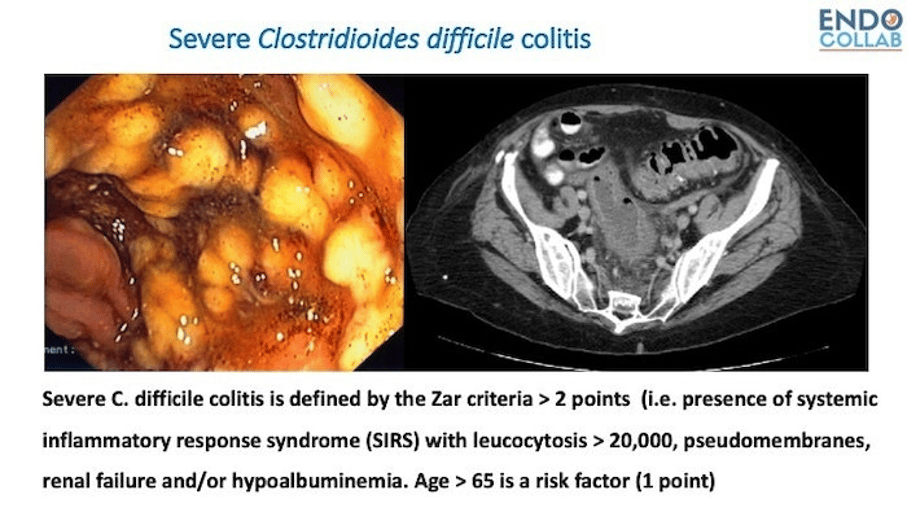
In clinical practice, all practicing endoscopists see and treat patients with C. difficile infection (CDI). One of the criteria for the severity of CDI is leukocytosis (1). Indeed, the leukocytosis in CDI can be so bad, that occasionally it’s called “leukemoid reaction”.
Let’s look at two classic clinical studies evaluating this issue. In a prospective study looking conditions associated with leukocytosis in hospitalized patients Wanahita et al found that of 53% of 400 inpatients with WBC counts of more than15,000 cells/mm3 had infection (2). Of these 207 patients, 97 (47%) had pneumonia, 60 (29%) had urinary tract infection, 34 (16%) had soft-tissue infection, and 34 (16%) had C. difficile infection. Importantly, CDI was present in 25% of patients with WBC counts of >30,000 cells/mm3 (2). In another prospective study looking into patients with unexplained leukocytosis, C. difficile infection was found to be the main culprit (3)
How does C. difficile cause leukocytosis?
During physiological circumstances, 95% of granulocytes reside in the bone marrow. Of the neutrophils in the blood half are circulating and half are marginated (4). Stress induces marinated granulocytes to enter the main circulation. Soon after toxin exposure in the colon, lots of neutrophils migrate there. Although a significant number comes from demarginalization, most originate from the bone marrow. How? We know that under basal conditions granulocyte colony-stimulating factor (G-CSF) is an essential regulator of neutrophil release from the bone marrow (5). In an elegant study looking into inpatients with CDI, asymptomatic carriage, or non-CDI diarrhea the investigators found that CDI lead to significant higher increase of cytokines (IL-1, IL-6, TNF-alpha) and G-CSF (granulocyte colony stimulating factor), as compared to non-CDI patients.
So, it’s this extra secretion of G-CSF that stimulates the bone marrow to release granulocytes and move them to the circulation, often causing a leukemoid reaction.
If you encounter patients with leukocytosis, think of CDI, and if they have CDI, let’s watch out closer, as these patients have a higher risk of complications.
References:
1. Zar FA, Bakkanagari SR, Moorthi KM, Davis MB. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007 Aug 1;45(3):302-7. doi: 10.1086/519265. Epub 2007 Jun 19. PMID: 17599306.
2. Wanahita A, Goldsmith EA, Musher DM. Conditions associated with leukocytosis in a tertiary care hospital, with particular attention to the role of infection caused by clostridium difficile. Clin Infect Dis. 2002 Jun 15;34(12):1585-92. doi: 10.1086/340536. Epub 2002 May 23. PMID: 12032893.
3. Wanahita A, Goldsmith EA, Marino BJ, Musher DM. Clostridium difficile infection in patients with unexplained leukocytosis. Am J Med. 2003 Nov;115(7):543-6. doi: 10.1016/s0002-9343(03)00420-0. PMID: 14599633.
4. ATHENS JW, RAAB SO, HAAB OP, MAUER AM, ASHENBRUCKER H, CARTWRIGHT GE, WINTROBE MM. Leukokinetic studies. III. The distribution of granulocytes in the blood of normal subjects. J Clin Invest. 1961 Jan;40(1):159-64. doi: 10.1172/JCI104230. PMID: 13684959; PMCID: PMC290701.
5. Semerad CL, Liu F, Gregory AD, Stumpf K, Link DC. G-CSF is an essential regulator of neutrophil trafficking from the bone marrow to the blood. Immunity. 2002 Oct;17(4):413-23. doi: 10.1016/s1074-7613(02)00424-7. PMID: 12387736.
Kelly CP, Chen X, Williams D, Xu H, Cuddemi CA, Daugherty K, Barrett C, Miller M, Foussadier A, Lantz A, Banz A, Pollock NR. Host Immune Markers Distinguish Clostridioides difficile Infection From Asymptomatic Carriage and Non-C. difficile Diarrhea. Clin Infect Dis. 2020 Mar 3;70(6):1083-1093. doi: 10.1093/cid/ciz330. PMID: 31211839; PMCID: PMC82044

