The MIRacle Sign
The Practicing Endoscopist Newsletter
The Practicing Endoscopist is brought to you by EndoCollab.
Visit EndoCollab.com for more endoscopy education.
Adil S. Mir MD FACP; Klaus Mönkemüller MD, PhD, FASGE, FJGES
Virginia Tech Carilion School of Medicine, Roanoke, VA, USA
Upper gastrointestinal (GI) endoscopy or esophagogastroduodenoscopy (EGD) continues to be an extremely useful diagnostic tool for perspicuous macroscopic findings. Besides, attention to detail remains of utmost significance in deciphering clinical clues to rather uncommon pathophysiology. Herein, we describe an observation and endoscopically inducible sign which could be a potential clue to diagnose borderline or overt gut ischemia.
We describe the case of an 81-year-old male patient with pertinent history of multiple medical comorbidities including gastroesophageal reflux disease, coronary artery disease, hypertension, diabetes mellitus, hyperlipidemia, congestive heart failure and history of deep venous thrombosis. Pertinent surgical history included the history of gastric volvulus requiring laparoscopic para-esophageal hernia repair and percutaneous endoscopic gastro-jejunostomy (PEG-J) tube placement about 1 month prior. The patient was admitted for the management of generalized weakness, nausea, electrolyte abnormalities, poor oral intake, and dehydration after he accidentally dislodged his PEG-J tube. After detailed risk and benefit discussions, the GI team was consulted, and the patient underwent endoscopic replacement of the same with gastropexy and placement of two suture-stays. Pertinent findings during EGD included scar at the previous gastrostomy site, fundic gastritis with/and likely worsened by retention of gastric contents, and severe reflux esophagitis (LA grade D).
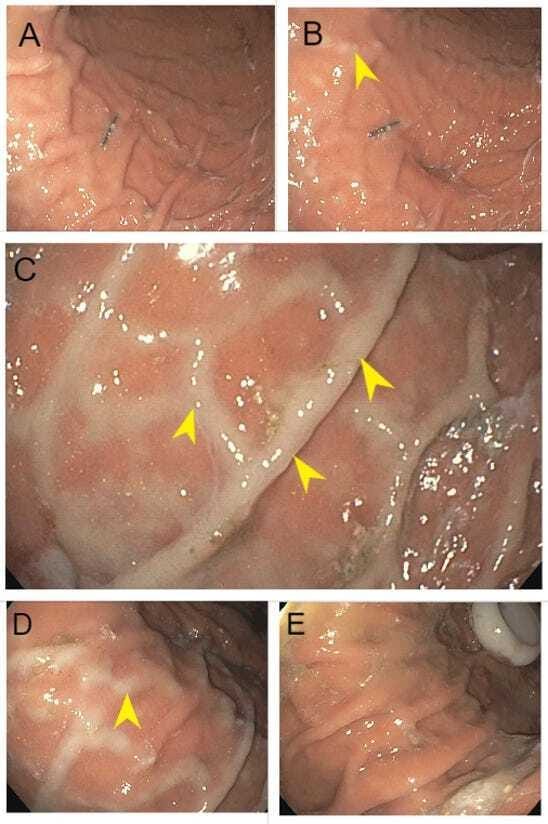
During the procedure, on entering the stomach with the standard EGD scope, the mucosa was noted to be grossly normal appearing and well perfused (Image 1: A). It was noted that progressive inflation of the stomach lead to sequential increasing pallor which was more pronounced at the top of the gastric mucosal folds (Image 1: B, C, D respectively). After the PEG tube was placed and the stomach decompressed, the gastric folds were noted to return to the normal appearing perfused salmon-pink mucosal color (Image 1: E). Carbon dioxide was used for inflation during this procedure. Throughout the procedure the patient’s vitals remained stable, without any documented hypotension..
Image 1: (A) Normal appearing perfused gastric mucosa on entering the stomach with an EGD scope; (B) Minimal blanching starts to appear (arrowhead); (C) Mucosal blanching with gastric inflation most pronounced on the top of the gastric folds (arrowhead); (D) Blanching starts to improve with deflation (arrowhead); (E) Blanching resolved with full deflation after completion of the procedure.
This ‘miraculously’ inducible phenomenon of reversible blanching of the gastric mucosa, most conspicuous at the top of the mucosal folds, appearing with inflation and disappearing with deflation, during the same procedure remains of clinical interest. We intend to give this sign the name of a miracle ‘The MIRacle sign’ after the name of the coining author.
Although gastric mucosal pallor or white mucosa during endoscopy has been described as a potential pointer to a diagnosis of chronic mesenteric ischemia, the phenomenon of endoscopic inducibility and reversibility during the same exam has not been described in detail [1,2]. Eliciting this sign during endoscopy should prompt the clinician to work up further causes of gastric/intestinal ischemia especially in patients with pertinent vascular history. Cross sectional imaging with angiography should be considered in such cases.
One of the very few signs that are inducible during endoscopy, such as esophageal rings in reflux and eosinophilic esophagitis or “cat scratch colon” in collagenous colitis, the MIRacle sign may potentially serve as an important diagnostic pointer in the appropriate patient population. It is possible that in a susceptible patient with underlying significant vascular or cardiac disease, progressive gastric inflation with carbon dioxide or air may transiently compromise the blood supply of the already borderline perfused stomach. We theorize this may either happen by virtue of microvascular compression from increased intragastric pressure or potentially worsening the take-off angle of the major vessels arising from the aorta, or both. Of course, whitening of the mucosa may appearduring epinephrine injection, but it is a patchy phenomenon, and it does not appear and disappear during endoscopy.
The MIRacle sign may further potentially serve as an indirect sign for the assessment of gastric vascular perfusion. Further studies are needed to determine and describe the scientific basis of this rather intriguing and puzzling phenomenon.
References:
Tsay CJ, Protiva P. Chronic Mesenteric Ischemia with Peristaltic Blanching. Am J Gastroenterol. 2021 May 1;116(5):870.
Ichita C, Sasaki A, Isogai N, Sumida C, Nishino T, Kubota J, Shionoya K, Kimura K. White gastric mucosa during endoscopy as a new endoscopic feature of chronic ischemic gastritis: A case report. DEN Open. 2022 Dec 13;3(1):e192.