Ulcerations of the Intestines in Patient with Multiple Endocrine Neoplasia (MEN) Type 2b
Presented by Prof. Adrian Canavesi:
Middle-aged patient 42 with MEN IIb syndrome, s/p thyroidectomy about 10 years ago for medullary thyroid cancer, s/p bilateral adrenalectomy due to pheochromocytoma one year later. Since then, taking hydrocortisone and fludrocortisone. About 5 years underwent subtotal colectomy due to intestinal obstruction and megacolon. Immunohistochemistry was performed, being positive for S100, which was diagnostic of intestinal ganglioneuromatosis.
She was recently admitted due to hematochezia but no abdominal pain, no fever, no weight loss, no night sweats.
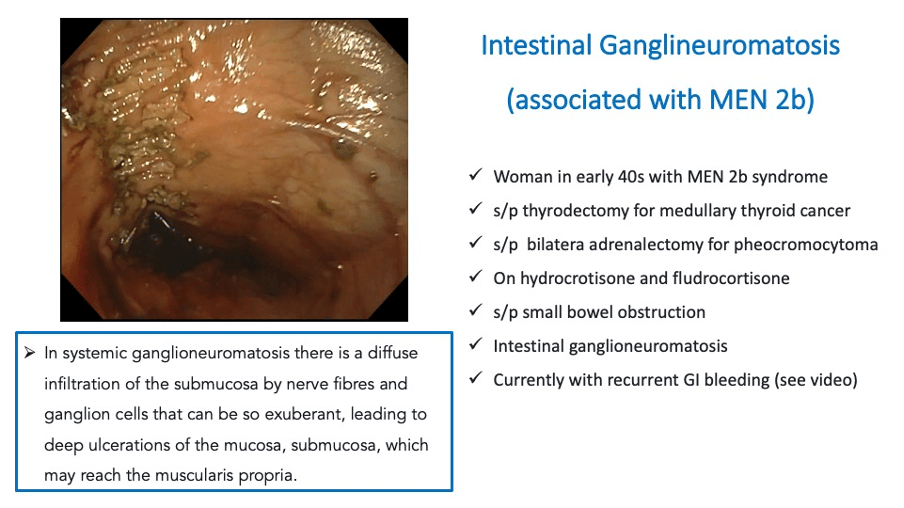
Push enteroscopy was unremarkable. However, ileocolonoscopy to 60 cm proximal to the ileocolic anastomosis shows dilated small bowel with multiple ulcers between 5 and 30 mm that tend to converge in some sectors, with congested edges and a deep bottom with fibrin; healthy surrounding mucosa.
What is your differential diagnosis?
Discussion by Klaus Mönkemüller:
Diffuse intestinal ganglineuromatosis can present sporadically or in association with von Recklinghausen disease (neurofibromatosis) or MEN2b, such as in your case.
The salient aspects of these ulcers are their depth and location. In cases of intestinal or colonic atonia or paralysis one must always think of stasis-ulcers (similar to stercoral ulcer). The location and linearity of the lesions also remind me of Zuckerberg or colon single strip sign (CSSS) in ischemic colitis, including the type associated with ingestion of NSAIDs, although these ulcers are in the small bowel. Thus, NSAID-induced ulcers must be ruled out.
Deep ulcers also should make one think of cytomegalovirus colitis, or tuberculosis, especially in a patient who is immunosupressed or taking steroids. Crohn's disease is always a consideration when small bowel ulcers are present, and also CMUSE (cryptogenic, multifocal ulcerative and stenosing enteritis).
MEN 1 is usually associated with gastrinoma, gastric hyperchloridia and diffuse small bowel ulcers. MEN2b is not generally associated with gastrinoma, but it is associated with hyperrparathroidism, which in turn leads to gastric hypersecretion, and eventual enteric ulcers.
Lastly, in systemic ganglioneuromatosis there is a diffuse infiltration of the submucosa by nerve fibres and ganglion cells that can be so exuberant, leading to deep ulcerations of the mucosa, submucosa, which may reach the muscular propria. I think this will be the final diagnosis in this case.
Biopsies will be very important, of course including special stains for cytomegalovirus, tuberculosis and nerve and spindle cells (e.g. calretinin, synaptophysin, S-100).
In addition, would obtain serum tests for tuberculosis (quantiferon), parathyroid-hormone (PTH) level, calcium, skin PPD, chest x-ray.
A CT of the abdomen or MRI would be helpful to determine the amount of transmural inflammation, extent of the disease, and presence or absence of lymph nodes.
Final Diagnosis: infiltrating intestinal ganglioneuromatosis.
New Lecture on EndoCollab
Rendezvous PTCD - Device-Assisted Enteroscopy ERCP
EndoCollab
✅ 1000+ endoscopy strategies
✅ 900+ endoscopists
✅ EndoCollab community to ask your questions
✅ No obligations, no contracts, CANCEL ANYTIME


